[Weekender] From lockdown to holiday visits, one nursing hospital’s COVID-19 journey
‘Slowly, things are changing for the better’
By Kim ArinPublished : Dec. 31, 2022 - 16:01
Some sense of normal life is returning to South Korea’s hospitals for the oldest and the most vulnerable patients.
Last weekend, Misodle Hospital for the elderly in Guro-gu, southern Seoul, spent the first Christmas since COVID-19 with in-person visits.
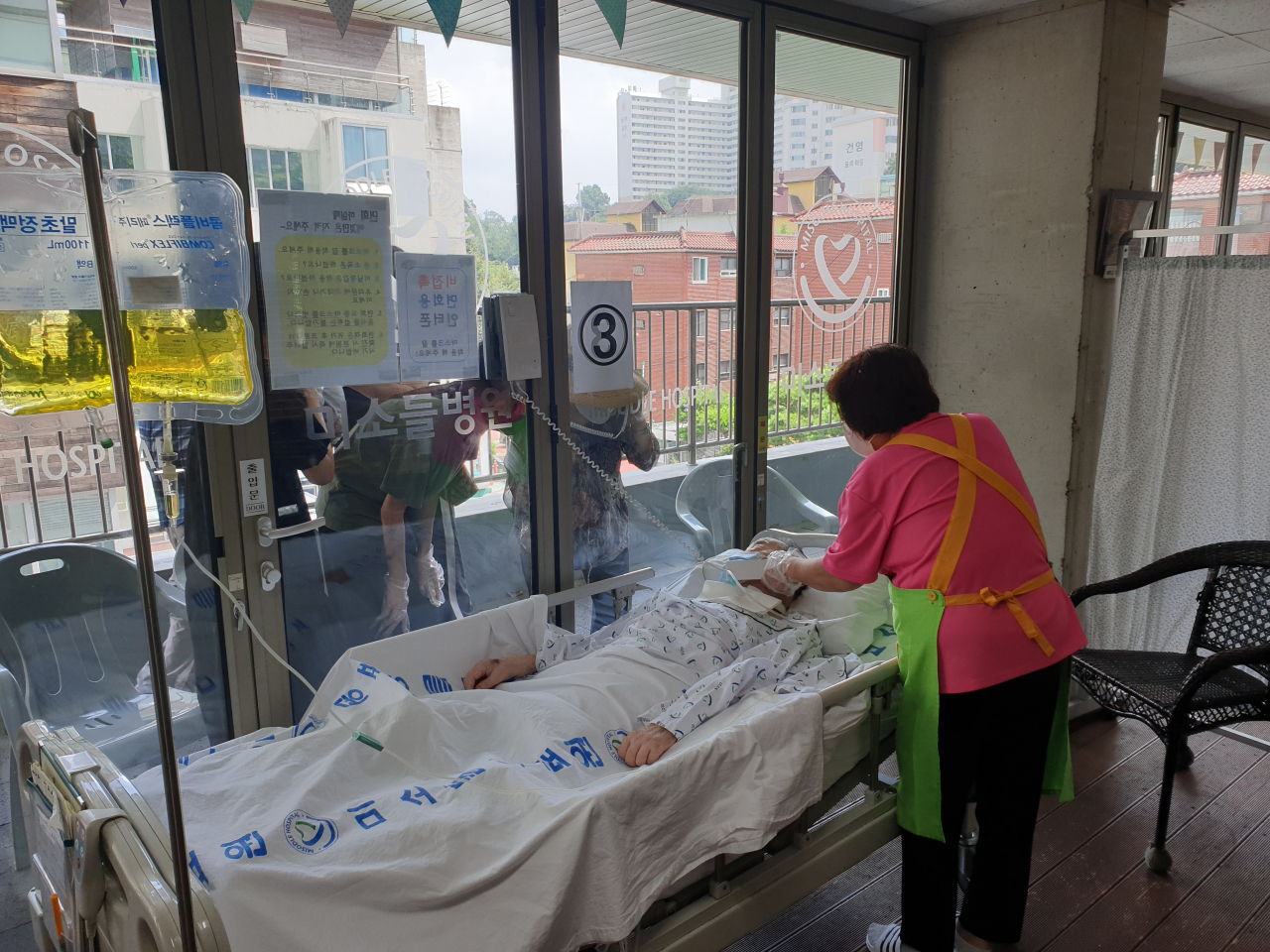
With social distancing and other rules already lifted, the government permitted face-to-face encounters at elderly care facilities from October. Up until this point, residents and visiting loved ones could only meet separated by a glass wall, as at many other nursing homes and hospitals.
"They had to speak over the phone. Sometimes they would say nothing and just cry,” said Wee Ji-young, a nurse of 20 years at Misodle.
Exceptions were only allowed when a resident was close to death.
“Even then the visitors had to dress in full personal protective equipment,” she said. “So they couldn’t really touch or hold one another.”
At least for now, Misodle is enjoying a respite after agonizing days of the strictest restrictions.
The hospital’s staffers still refrain from traveling or even dining at restaurants. If they’d been to crowded places, they would take a test before returning to work to make sure they’re negative. Wee said many on the staff exercised these precautions voluntarily, even after they were no longer required.
While things haven’t returned to the way it was before, many employees spent the holiday with their families and “enjoyed some normalcy” for the first time in a long time.
Two winters ago, Misodle Hospital became a COVID-19 island with no exit.
The entire hospital was placed under what is known as “cohorting” -- when a group of people are locked down following exposure -- for over a month, which “felt like forever” to the patients and medical workers who lived through it.
On Dec. 15, 2020, a patient at the hospital tested positive for COVID-19 for the first time. The hospital was immediately forced into lockdown in accordance with the then-government protocol for elderly care facilites. All of the hospital’s patients and staff -- with or without COVID-19 -- were locked down together indefinitely until the outbreak subsided. For dozens of patients, death became the only way out.
Misodle, as a convalescent hospital, was not equipped to treat COVID-19. Patients died without receiving the treatment they needed or being able to see family. Some of the patients who died in lockdown did not have COVID-19, but they still were not able to leave until their last day. One medical worker at the time described it as “being quarantined to death.”



Nurses and care workers were sleeping on the floor and working under hazmat suits for 12 to 15 hours a day. Ten nurses were looking after about a hundred patients at the ward Wee was at.
“I remember video-calling with my family, they were so worried,” she said.
COVID-19 “spread like wildfire” at the hospital. It took only about a week for one case to become a hundred. Over the 42-day lockdown, 167 were confirmed with COVID-19 -- 95 of them patients and the rest medical workers and other employees at the hospital. All of them had to wait for beds to free up at hospitals that provide COVID-19 treatment.
A string of outbreaks at nursing homes and hospitals nationwide, which led to more than 500 deaths between mid-December 2020 and early January 2021, had filled beds nationwide.
At the end of the lockdown on Jan. 25, 2021, the death count at Misodle stood at 54. Less than half -- 25 -- of those deaths were associated with COVID-19. The other 29 never tested positive.
Even for this hospital for the elderly, 29 deaths in 42 days is “unusually high,” said an official at the hospital who did not want to be identified.
“The lockdown must have taken a toll. We saw about 1.5 to 2 times our usual number of deaths,” the staffer said.
In the midst of the lockdown that barred every member of the Misodle community from going home, one of the medical workers submitted an online petition to the Cheong Wa Dae website.
“COVID-19 patients are dying waiting to be moved to a different hospital. They’re not getting treated after a positive test. Non-COVID-19 patients are also dying. Nurses are getting sick looking after patients, and becoming patients themselves. All of us are very scared. We’re just waiting for help to arrive,” read the petition dated Dec. 27, 2020.
But Misodle was “pretty much on its own,” according to the hospital official. There were some COVID-19 medical products supplied to Misodle by the public health office, like personal protective equipment, but the hospital had to buy “nearly 90 percent” of what it needed. Although the lockdown was a government policy, the hospital was not reimbursed.
Dr. Yoon Young-bok, Misodle’s director and the head of the country’s association of geriatric hospitals, said he “lived at the hospital” as long as the lockdown persisted. He said some 70, which is about half of the medical staff, quit afterward.
“I couldn’t blame them. They’d gone through so much,” he said. “There were some who gave up because they were so afraid of the disease. We didn’t know much about it then.”
The hospital “has never quite rebounded” since, he said. After the post-lockdown exodus of workers, it was hard to find new workers who could replace them.
There was also the emotional trauma.
“You never fully recover from something like that,” he said.
Misodle rose from its painful lockdown into a full-time COVID-19 hospital. Over a year and a half until May, the hospital took in some 4,400 patients with moderate disease.
“At the time, we were the only nursing hospital with COVID-19 experience. We knew it wouldn’t be easy. Not everyone at the hospital was on board with the idea. But we also knew we would have a lot to contribute in the COVID-19 fight,” Yoon said.
The hospital tried to give up once, in September last year, when the government tried to cut relief funding. The government said it would not pay for the hospital’s COVID-19 beds and workforce.
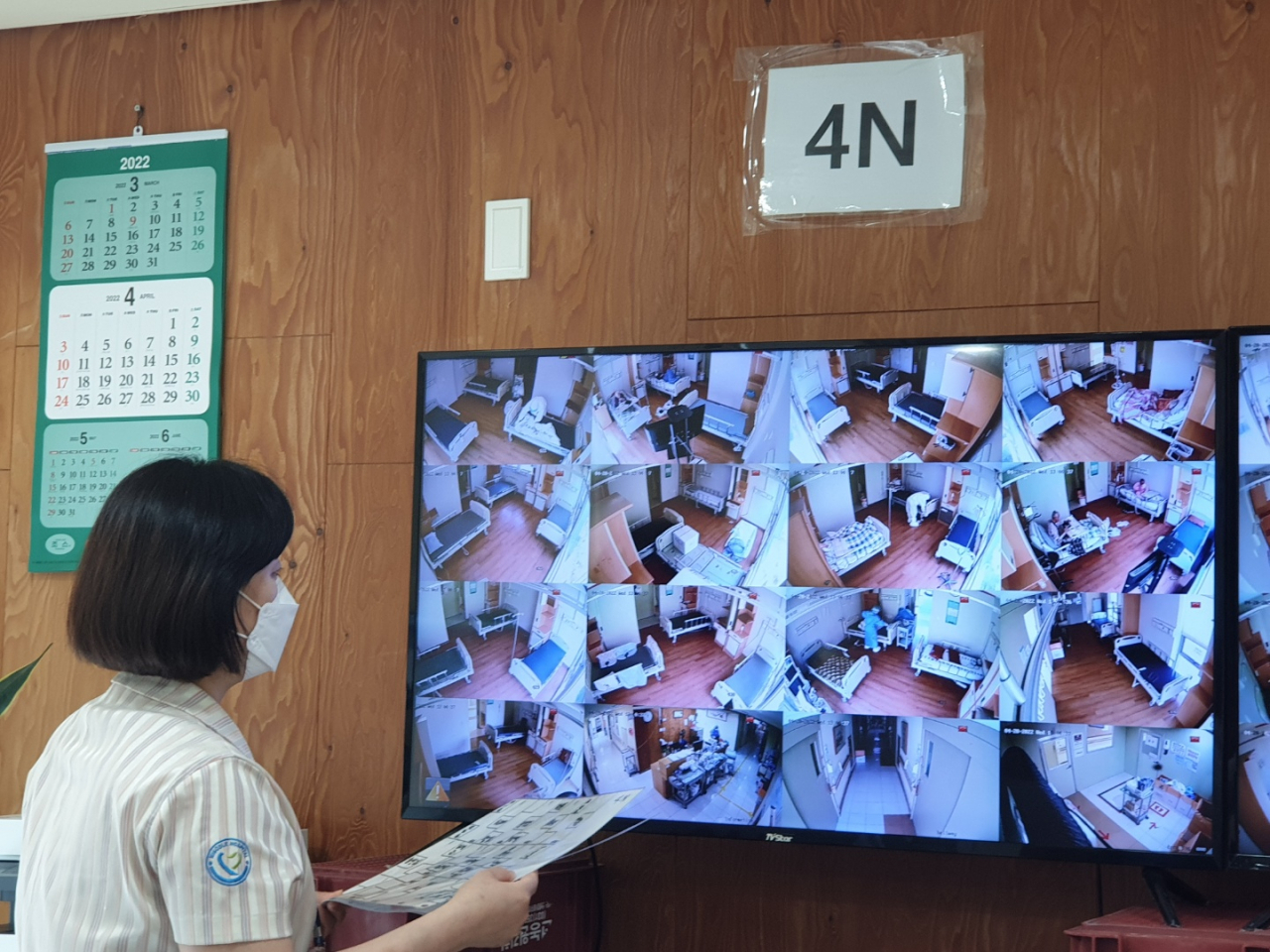
Some things have not changed. Just like the early days of the pandemic, all of the hospital’s staffers are tested weekly and every time they come down with suspected symptoms.
“Our staffers must have taken hundreds and hundreds of tests in the last few years,” he said.
Misodle also has staff members isolate for a week if they get COVID-19, much longer than the government-recommended three days for health care professionals.
“Because our patients are extremely vulnerable, we have to be cautious,” he said. “I think this is just the way things are going to be for a while.”
Still, the days of ultracaution seem to be in the past. More patients survive now than before. The hospital’s director said compared to the delta wave, patients were doing “much better.”
The hospital had Christmas trees and lights this year. For the last two Christmas celebrations the hospital was “so swamped with COVID-19, holiday was unthinkable,” he said.
“It doesn’t look like the virus will go away. But the pandemic is becoming more livable. Slowly, things are changing for the better.”


















![[Today’s K-pop] Treasure to publish magazine for debut anniversary](http://res.heraldm.com/phpwas/restmb_idxmake.php?idx=642&simg=/content/image/2024/07/26/20240726050551_0.jpg&u=)